 12 August, 2024
12 August, 2024
Complex LM PCI with Rotablation: A Step-by-Step Guide | Dr. AB Gopalamurugan
Coronary artery disease is a major health issue affecting millions worldwide. Among the various treatment options, percutaneous coronary intervention (PCI) has emerged as a key procedure for managing significant blockages in coronary arteries. This article delves into a complex PCI case involving rotablation, a technique used to treat heavily calcified lesions. We will explore the patient’s history, the procedural steps, and the outcomes of the intervention.
Patient Background
The patient is a 77-year-old man with a medical history of diabetes and hypertension. He presented with chest pain at a different hospital, where an abnormal ECG and positive troponin levels led to a diagnosis of non-ST elevation myocardial infarction (NSTEMI). An angiogram revealed significant double vessel disease impacting the left main coronary artery, left anterior descending artery (LAD), and right coronary artery (RCA).
Despite being advised to undergo a bypass operation, the patient preferred angioplasty. The left ventricular function was normal, with an ejection fraction (LVEF) of 60%. However, there were anterior wall motion abnormalities indicating that revascularization was necessary due to the patient’s ongoing symptoms.
Understanding the Angiogram
The initial angiogram showed critical disease in the left main artery, with significant calcification and a long segment of severe stenosis in the LAD. The circumflex artery appeared largely unobstructed, while the RCA had considerable mid-vessel disease. Given the complexity of the case, a careful approach was necessary to ensure successful intervention.
Procedure Preparation
The procedure began with a radial approach, but the radial artery was too small to accommodate a six French sheath. As a result, the team switched to the femoral access to ensure adequate support for potential rotablation. A six French JR 3.5 guide was used to treat the right coronary artery first, aimed at improving perfusion before addressing the left system.
Intervention on the Right Coronary Artery
During the intervention on the RCA, a 2.5 by 12 balloon was utilized to address the tough stenosis. High-pressure balloon inflation was necessary to achieve adequate expansion, with pressures reaching up to 24 atmospheres. A synergy stent measuring 2.5 by 38 was then deployed, followed by post-dilation with a 2.75 by 12 balloon to ensure optimal stent expansion.
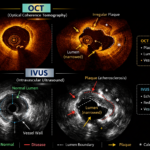
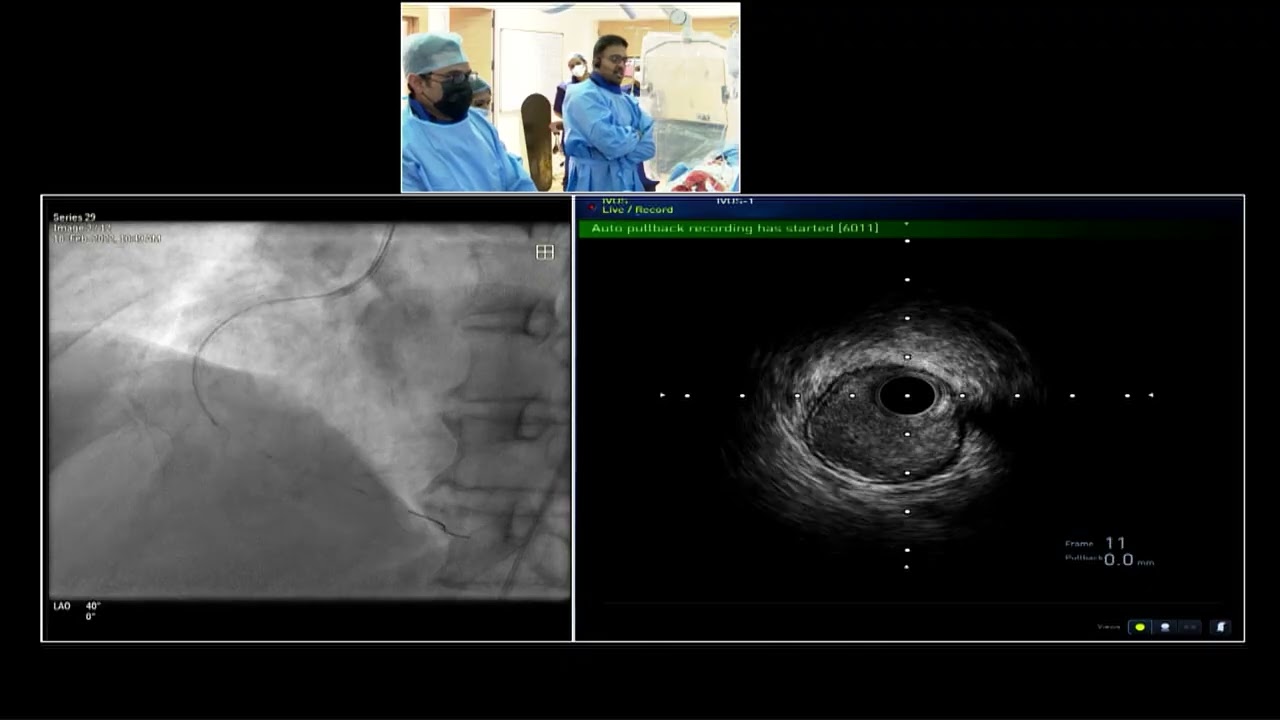
Intravascular ultrasound (IVUS) was employed to assess the results of the RCA intervention. The images revealed well-opposed stent apposition with no signs of under-expansion or malposition. The distal flow was satisfactory, indicating that the procedure had been successful in restoring blood flow through the RCA.
Transitioning to the Left System
With the RCA successfully treated, the focus shifted to the left system. A seven French EBU-35 guide was introduced to facilitate potential rotablation. The team was cautious while navigating the left main artery, given the significant calcification present.
Addressing the Left Main Lesions
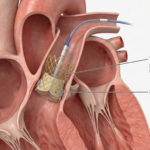
As the team prepared to perform rotablation, they observed a large chunk of calcium in the distal left main artery. To effectively debulk this calcium, a rota wire was introduced with a bias towards the LAD to maximize the churning effect of the rotablation burr. A 1.75 mm burr was selected for debulking, and the team proceeded with the rotablation technique.
The rotablation process involved careful monitoring for hemodynamic changes, as bradycardia was noted during the procedure. The team managed the patient’s condition by adjusting medication and ensuring proper flow through the coronary arteries. Following the successful debulking, the team prepared for balloon dilation to optimize the results.
Final Steps and Stenting
Once the rotablation was complete, a 2.5 by 12 balloon was used to dilate the narrowed segment in the LAD, resulting in significant lumen gain. The team then proceeded to stent the left main to LAD segment using two synergy stents: a 2.5 by 24 and a 3 by 16. The stents were carefully positioned, with a focus on minimizing overlap and ensuring adequate expansion.
Post-dilation with a 4 mm balloon was performed to ensure optimal stent apposition and to address any residual narrowing. Intravascular imaging confirmed excellent results, with the stents well opposed and no significant inflow pathologies noted. The overall lumen gain was impressive, demonstrating the efficacy of the combined rotablation and stenting approach.
Conclusion and Patient Outcome
The intervention was a success, with the patient experiencing significant improvement in coronary blood flow. By utilizing advanced techniques such as rotablation and intravascular imaging, the team was able to achieve optimal results without the need for surgical bypass. The patient was expected to recover well and be discharged within a few days.
This case highlights the importance of personalized treatment strategies in managing complex coronary artery disease. With the right approach and techniques, patients can receive effective interventions that improve their quality of life and reduce the risk of future cardiac events.
Key Takeaways
- Complex coronary interventions require a thorough understanding of the patient’s anatomy and disease severity.
- Rotablation is a valuable technique for treating heavily calcified lesions, allowing for effective stenting.
- Intravascular imaging plays a crucial role in ensuring optimal outcomes during PCI procedures.
- Patient preferences should be considered when determining the best course of treatment for coronary artery disease.