Insights on Laser Angioplasty, Rotablation, Orbital, & Lithotripsy in Complex Angioplasty india Rotablation in india
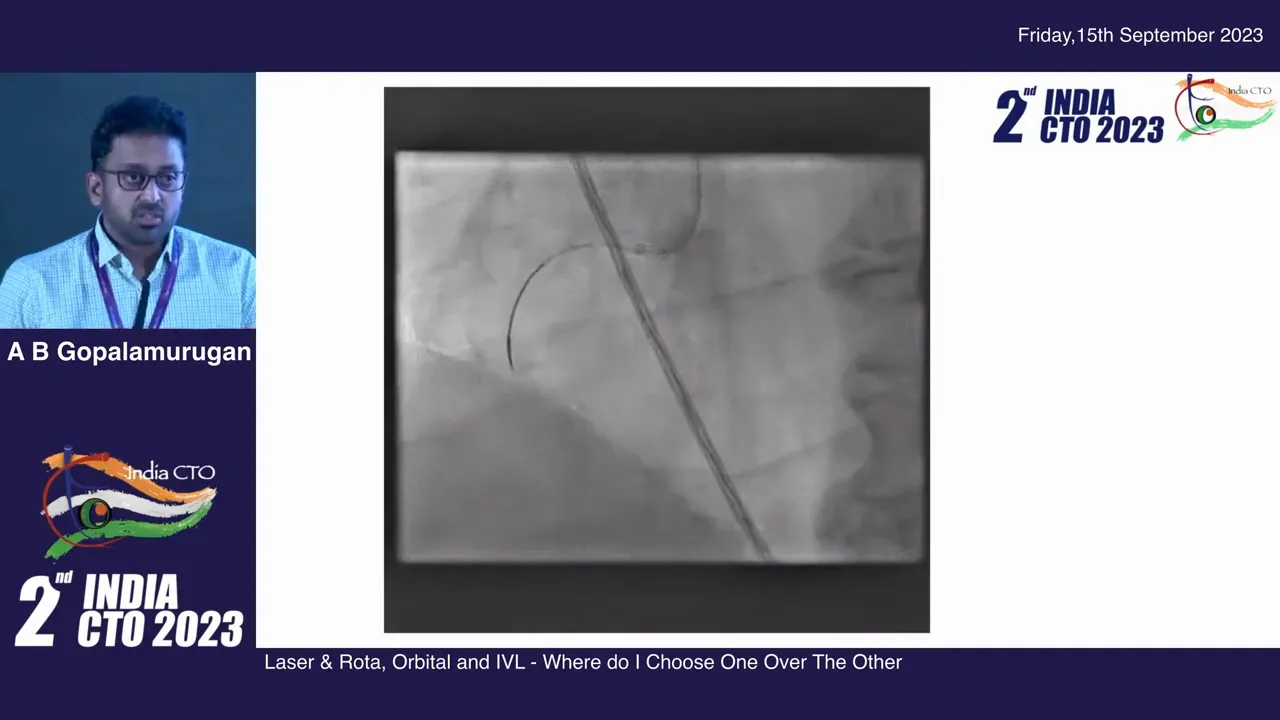
I presented this lecture at India CTO 2023 and in it I share my personal approach to complex lesion preparation — when to choose laser, rotablation, orbital atherectomy or intravascular lithotripsy. In this article I outline real-case examples, explain the rationale behind choosing one device over another, and provide practical procedural end points that guide my decisions. If you are involved in high-risk or heavily calcified percutaneous coronary interventions, especially Complex Angioplasty india Rotablation in india , this is a practical, experience-based guide
Table of Contents
- Outline
- Introduction
- Debulking versus Lesion Modification: Definitions and Why They Matter
- Case Example 1 — RCA with Nodular Calcific Lesion: Rotablation + Laser + Lithotripsy
- Why Use Laser First When a Device Won’t Cross?
- Case Example 2 — Predominantly Abluminal Calcification Treated with IVL
- Case Example 3 — Orbital Atherectomy for Guiding Catheter Size Constraints and Left Main Disease
- Instant Stent Restenosis — When Calcified Tissue Appears Within a Stent
- How I Decide — Procedural End Points That Drive Choice
- Practical Tips — How I Use the Devices
- Complication Avoidance and Troubleshooting
- Real Quotes and Pearls I Often Repeat
- FAQ
- Conclusion
Outline
- Introduction: why device selection matters in calcified lesions
- Definitions: debulking vs lesion modification
- Case examples and device strategies
- Stepwise decision-making and procedural end points
- Practical tips for combining devices
- Complication avoidance and troubleshooting
- FAQ
- Conclusion
Introduction
Complex coronary lesions often require more than balloon angioplasty and stent deployment. I frequently manage lesions where heavy calcification, nodules or chronic stent-related calcium make standard techniques inadequate. When I teach and when I treat, my goal is straightforward: achieve an optimal minimum stent area (MSA) with minimal residual flow turbulence and durable expansion. The phrase that keeps coming back in my practice is Complex Angioplasty india Rotablation in india — it reflects the reality that in India, and globally, complex PCI often requires advanced adjunctive technologies and tailored combinations.
In the next sections I will walk you through examples from my practice that illustrate when I choose rotablation (rotor), orbital atherectomy, excimer laser, intravascular lithotripsy (IVL), or combinations of these tools. I will also describe the thought process I use to decide which strategy is most likely to achieve the best MSA and long-term outcome — again, in the context of Complex Angioplasty india Rotablation in india .
Debulking versus Lesion Modification: Definitions and Why They Matter
Before diving into cases, let’s define two broad categories of devices so decision-making is explicit:
- Debulking technologies remove plaque material from the lumen. Examples: rotational atherectomy (rotablation) and orbital atherectomy. These devices abrade and remove material, creating more luminal area when used effectively.
- Modifier technologies change the mechanical properties of plaque without removing significant bulk. Examples: intravascular lithotripsy (IVL) and laser when used to disrupt calcific architecture. They create microfractures or vaporize softer tissue, allowing balloon expansion and stent deployment.
Understanding this distinction is critical. If your lesion needs material removed (a large nodular calcium or a stent sandwiching calcium), a modifier alone may not achieve the MSA required. Conversely, if the problem is predominantly abluminal concentric calcium without a large luminal nodule, modification (IVL or laser) may be enough and carries different risk profiles.
I emphasize this every time I plan a case of Complex Angioplasty india Rotablation in india — know whether you need to debulk, modify, or both.
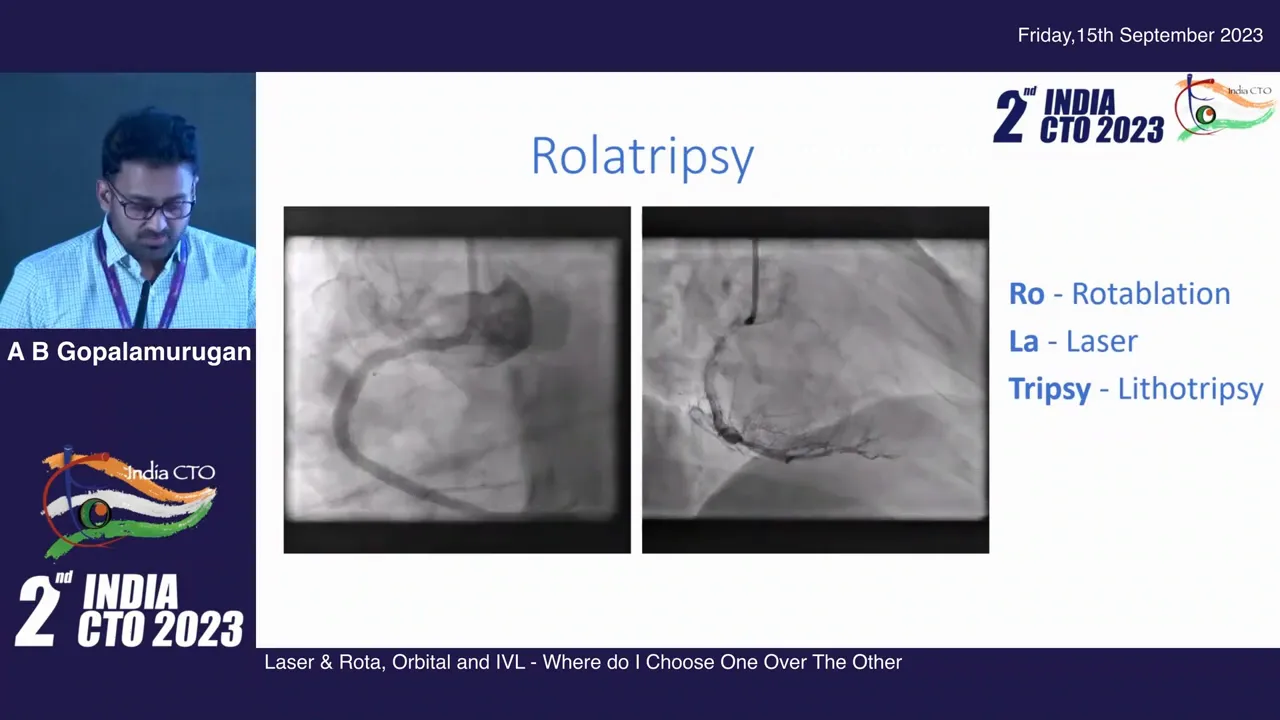
Case Example 1 — RCA with Nodular Calcific Lesion: Rotablation + Laser + Lithotripsy
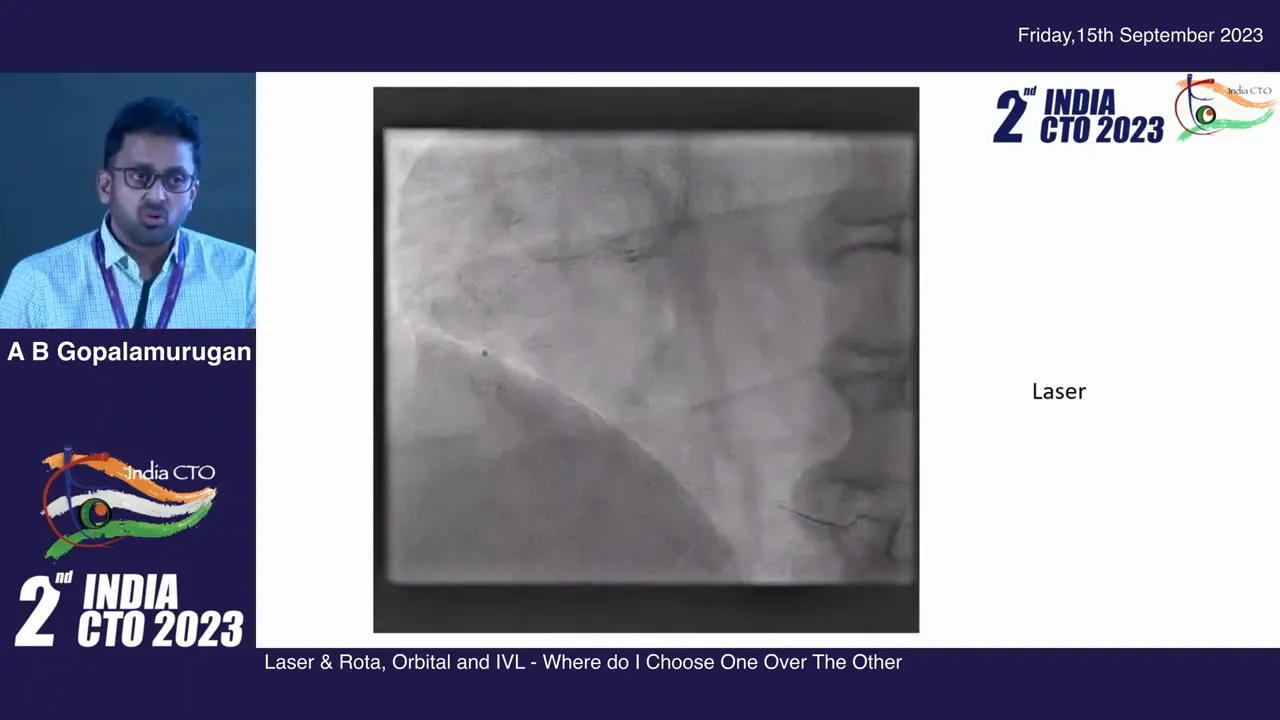
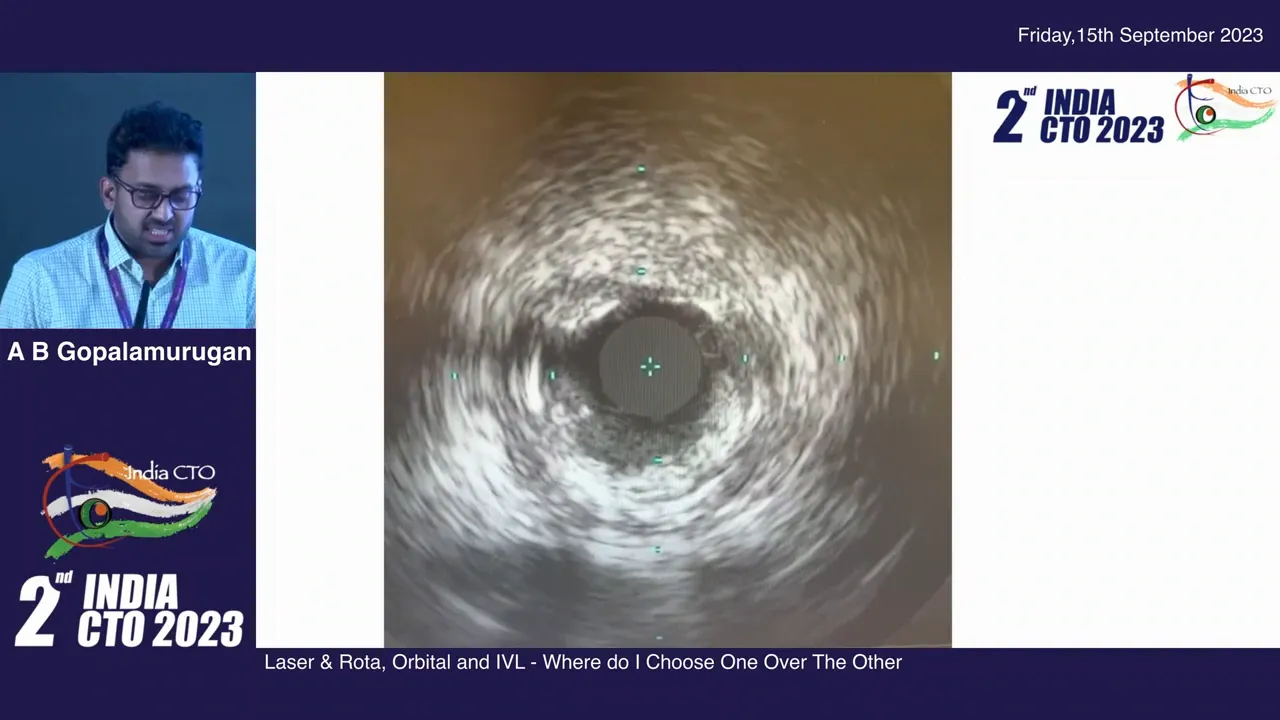
Let me describe a case that typifies when combination therapy is necessary. The angiogram showed an RCA with dense pilling defects and a nodular calcific lesion. Multiple guidewires were attempted and a balloon could not cross the lesion — a classic setup for rotablation. We managed to cross with a wire using balloon support, but a 1.25 mm center marker balloon would not advance despite good guide support.
At this point I gently dilated without causing dissection, remembering that a dissection would preclude safe rotablation. I wedged a microcatheter but it would not cross — the microcatheter was parked, wire exchanged and a rotawire passed. The rotawire advanced but the rotablation burr couldn’t cross initially. The patient had chest pain and no antegrade flow, so time and safety were paramount.
We elected to use an excimer laser catheter (an ELCA) — a key decision point. I typically choose laser when the wire has crossed but no device can, especially when the vessel is occlusive and the microcatheter cannot be advanced. Laser allowed us to create a channel and modify the lesion sufficiently to permit subsequent device passage. In this case, after laser modification a microcatheter and rotawire were advanced, and rotablation with a 1.5 mm burr followed, upsized later to 2.0 mm, given the degree of calcium.
Even after debulking there remained a resistant calcified nodule. Further mechanical debulking would not eliminate this nodule, so we used intravascular lithotripsy to create cracks in the remaining calcium (remember, lithotripsy is a modifier, not a debulker). After IVL, balloon expansion and stenting produced a very pleasing angiographic result.
This combination — rotablation, laser, lithotripsy — is common in my practice, and highlights important principles: when devices fail alone, staged and combined therapies often achieve the necessary MSA. This case is a prototypical example of Complex Angioplasty india Rotablation in india where multiple modalities are complementary.
Why Use Laser First When a Device Won’t Cross?
Laser is uniquely useful when the wire has crossed but no device can follow. Drilling, high-pressure ballooning or repeated small balloon attempts (and even grenadoplasty) can create dissections and compromise the vessel, sometimes forcing the patient to return another day. Laser can create a channel or sufficiently change the lesion so that microcatheter and atherectomy devices can be passed safely in the same sitting.
Remember: laser works best when you have wire access. It “vaporizes” soft tissue and creates pathways, but it is more of a modifier in calcified disease unless contrast-assisted lasing is used to create high-pressure microexplosions. Always consider vessel wall integrity and avoid aggressive lasing if dissection is suspected.
Case Example 2 — Predominantly Abluminal Calcification Treated with IVL
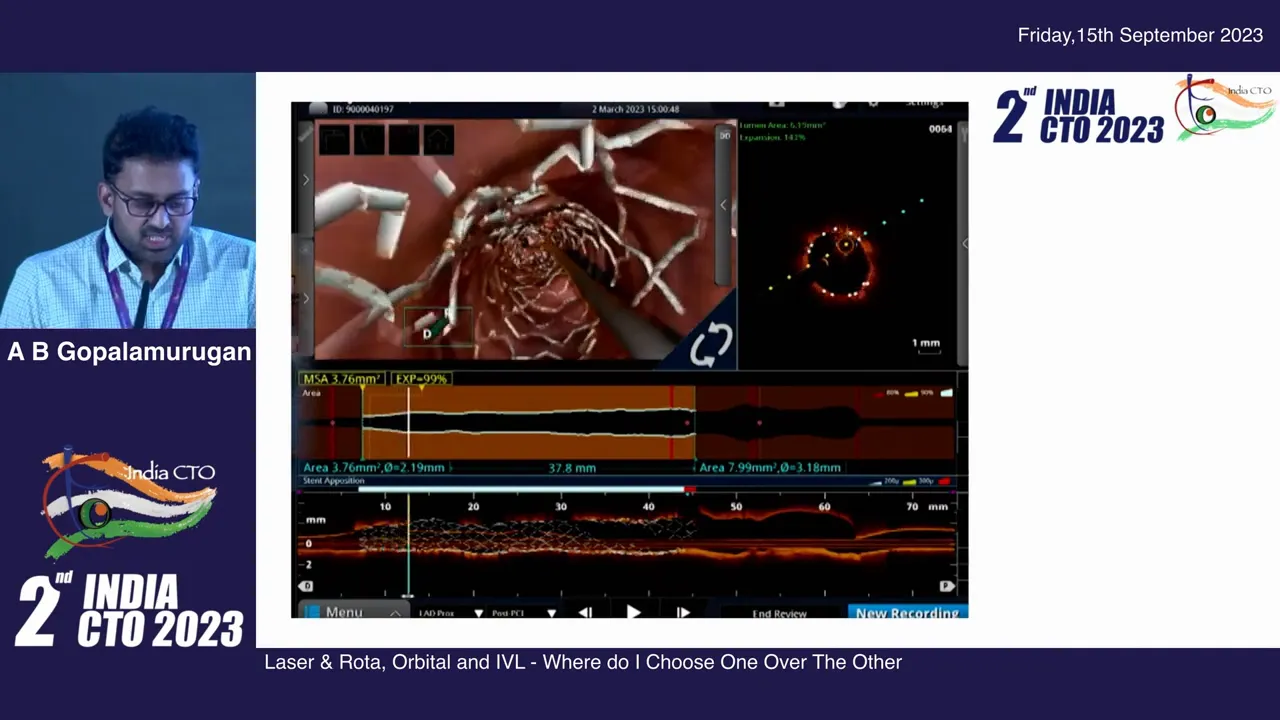
Not all lesions need debulking. I treated a patient whose calcium burden was mostly abluminal; the lumen appeared relatively spared. IVUS would have shown minimal luminal superficial calcium in some lesions — in these cases IVL can be highly effective. For this patient, several rounds of lithotripsy were required — we delivered four IVL balloons at the same proximal location, exhausting pulses to crack the deep calcium and allow balloon and stent expansion.
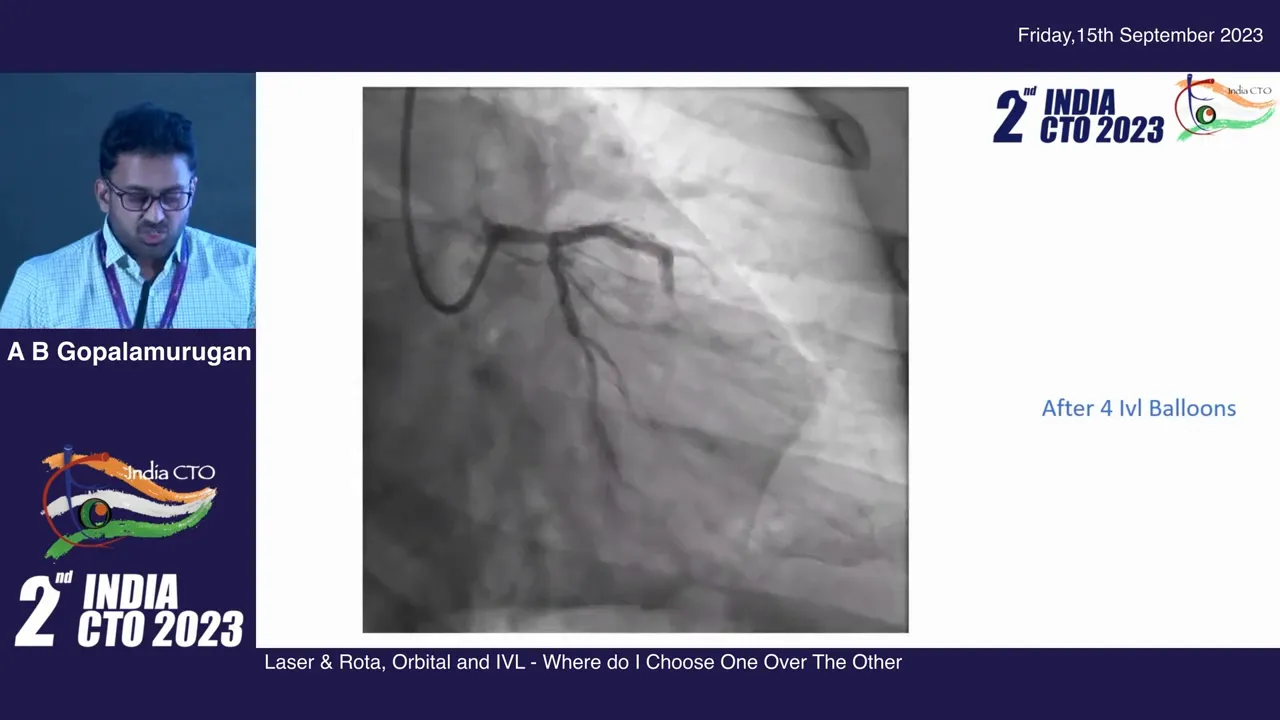
After the IVL sessions the lesion yielded and permitted stent deployment with an excellent angiographic result. This demonstrates that IVL is a powerful lesion modifier when the goal is to change the compliance of deep, concentric calcium rather than remove tissue.
Again, in the setting of Complex Angioplasty india Rotablation in india , IVL is a practical first-line tool for purely abluminal calcium where debulking may be unnecessary.
Case Example 3 — Orbital Atherectomy for Guiding Catheter Size Constraints and Left Main Disease
Sometimes logistical factors such as guide size determine the choice. In one case we began with a 6F guide and did not want to upsize. To achieve a larger lumen area without upsizing we turned to orbital atherectomy. Orbital can achieve effective debulking and can often produce a 2.0 mm lumen when used longer and with sufficient passes. In this patient we debulked with orbital and finished with IVL to treat abluminal calcium, finally reconstructing a dual ostial left main bifurcation with a very satisfying result.
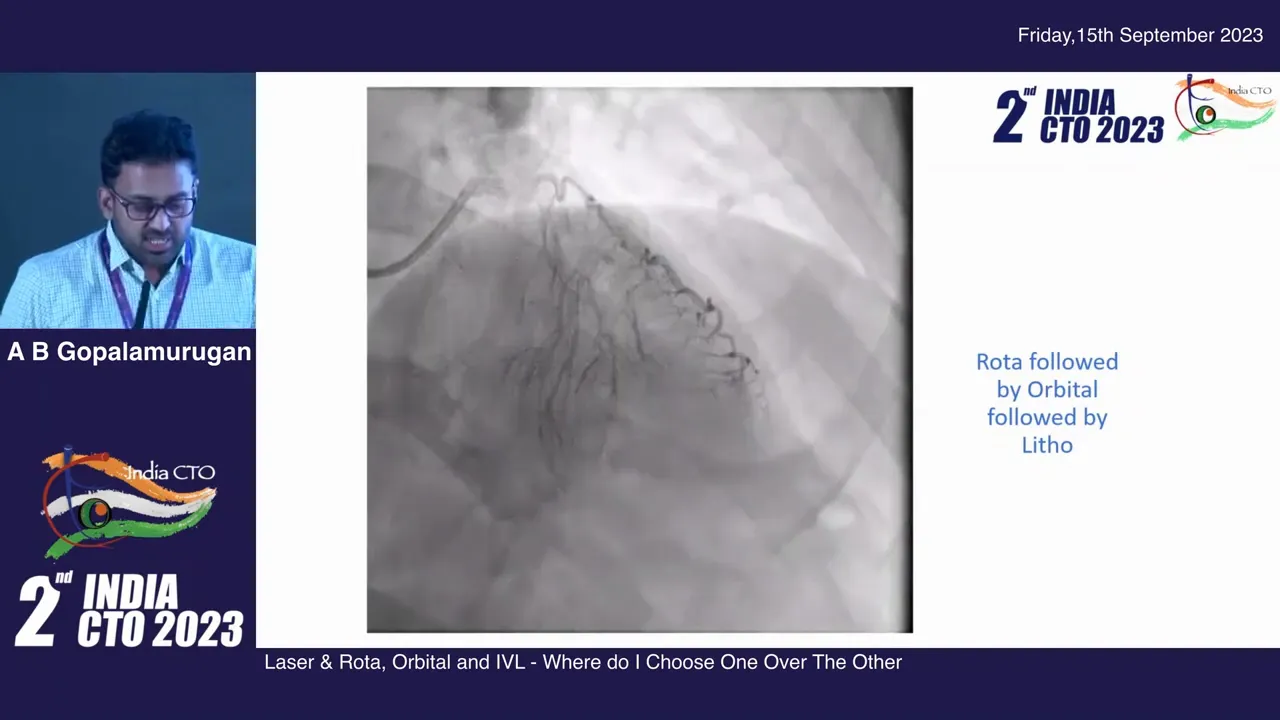
Orbital atherectomy was our debulker and IVL the modifier — an effective example of combining technologies when vessel and procedural constraints exist. Again, this is an illustration of Complex Angioplasty india Rotablation in india where flexibility in device selection matters.
Instant Stent Restenosis — When Calcified Tissue Appears Within a Stent
Instant restenosis can be “juicy” tissue that you can cut away with a cutting balloon or even a scoring balloon. But sometimes instantaneous restenosis is calcific. I recall a 14-year-old stent with severe calcific in-stent tissue on IVUS. The calcific component meant that if we simply dilated and re-stented, the calcium would be sandwiched between stents — making it unlikely to achieve an adequate MSA.
Given we were on a 6F platform, we chose orbital atherectomy despite a relative contraindication for atherectomy inside stent geometry. In chronic stents that are endothelialized, the risk is lower and orbital can effectively debulk. We spent time ensuring the orbit achieved a mean luminal diameter of approximately 2.0 mm before proceeding with a new stent. The final imaging showed a good stent area and a favorable angiographic result.
In my practice, the answer to in-stent calcific instant restenosis often falls into the realm of Complex Angioplasty india Rotablation in india — if you cannot achieve MSA with modification alone, consider careful debulking where safe.
How I Decide — Procedural End Points That Drive Choice
My decision-making is focused on endpoint-driven goals rather than device dogma. I ask:
- What minimum stent area (MSA) do I need based on vessel size? Achieving a true MSA is the most important predictor of durable results.
- Is there a luminal nodule that will create flow disturbance if not removed? Big nodules predispose to early target lesion revascularization if left untreated.
- Is the calcium predominantly abluminal (deep) or luminal (superficial/nodular)? Abluminal calcium often responds well to IVL; luminal nodules may need debulking.
- Are we limited by guide size or access? If we must stay on a small guide, orbital may be preferred for debulking capacity without upsizing.
- Is there an old stent or scaffold involved? In-stent calcified tissue often requires debulking rather than modification alone.
If the expected MSA with a modification-only strategy is inadequate, I will lean toward debulking. If modification alone will achieve the MSA, particularly for concentric deep calcium, IVL is often my choice. If neither alone suffices, combination therapy is the practical solution.
Practical Tips — How I Use the Devices
- Always start with intravascular imaging when feasible. IVUS or OCT helps distinguish luminal nodules from abluminal calcification and guides device choice.
- If the wire is across but microcatheter or balloons cannot be delivered, consider laser (ELCA) to create a channel before attempting heavy mechanical debulking.
- When using rotablation, avoid creating dissections before atherectomy; gentle predilation is okay but severe dissection precludes safe rotablation.
- Orbital atherectomy can be used through smaller guides and is valuable when you must avoid upsizing; allow sufficient passes to achieve desired lumen size and be patient — time matters.
- IVL is powerful for deep calcium but is a modifier: you may need multiple balloon deliveries at the same site to exhaust pulses and get full effect.
- Combine modalities when a single technology cannot achieve the required MSA. For example: laser to enable crossing, rotablation or orbital to debulk, then IVL to finish abluminal calcium cracks.
These practical points have been refined through many cases of Complex Angioplasty india Rotablation in india — experience teaches when to escalate and when to combine.
Complication Avoidance and Troubleshooting
Complex interventions carry risks. Key strategies to minimize harm:
- Monitor for ischemia during prolonged device use — many of these procedures temporarily limit flow.
- Avoid aggressive lasing or atherectomy in presence of major dissections or perforation risk. If dissection occurs, reassess strategy immediately.
- When performing atherectomy inside a stent, understand this is relatively contraindicated but sometimes necessary in chronic endothelialized stents — proceed cautiously and document justification.
- Use embolic protection selectively in high-risk thoracoabdominal or peripheral cases, though rarely used in coronary work.
- Be prepared with bailout devices: covered stents, microcatheters, and support wires. Team readiness is vital.
These precautions are part of my everyday practice of Complex Angioplasty india Rotablation in india — safety is as important as technical success.
Real Quotes and Pearls I Often Repeat
“My procedural end points for all PCIs that determine what I choose is largely based on what’s the best MSA or minimal lumen diameter I want to achieve.” — Dr. A B Gopalamurugan
That sentence guides everything. If a chosen strategy cannot produce the MSA required for the vessel, change strategy. This pragmatic, endpoint-driven approach prevents unnecessary incremental attempts and improves long-term outcomes.
FAQ
Q: When should I pick laser over atherectomy?
A: Use laser when the wire is across but no device or microcatheter can be passed. Laser can create a channel and enable subsequent debulking or balloon delivery. In heavily calcified luminal nodules laser alone is unlikely to be sufficient — it is most helpful as an enabling tool. For complex cases labeled Complex Angioplasty india Rotablation in india , laser often plays a bridging role.
Q: Is IVL ever a standalone therapy?
A: Yes—if IVUS/OCT shows mostly abluminal concentric calcium and the predicted MSA after IVL is acceptable, IVL alone can be effective. However, if there are large luminal nodules or in-stent calcific tissue, IVL may not achieve adequate MSA without adjunctive debulking.
Q: How do you choose between rotational and orbital atherectomy?
A: Both are debulking devices. Rotablation is well-established for nodular calcified lesions and CTO scenarios. Orbital atherectomy can be advantageous when guide size limits upsizing because it can be effective through smaller guides and provide circumferential sanding. Device handling preferences and operator experience also play a role. In my practice, Complex Angioplasty india Rotablation in india often uses both at different times depending on access and lesion morphology.
Q: Is atherectomy safe inside a stent?
A: Atherectomy inside a stent is generally contraindicated due to the risk of device-stent interaction and embolization. However, in chronic, fully endothelialized stents with significant calcific in-stent restenosis, cautious orbital atherectomy may be considered as a relative exception. Proceed with extreme caution, document rationale, and consider imaging guidance.
Q: How many IVL pulses do you deliver at one site?
A: It depends on response; sometimes a single balloon (with limited pulses) is enough, but other times I deliver multiple IVL balloons and exhaust pulses at the same location (as in my case where four balloons were needed) to achieve adequate modification. Monitor balloon compliance and imaging feedback to guide the number of pulses.
Conclusion
There is no single device that handles every calcified or complex lesion. In my experience, treating complex coronary disease requires an endpoint-driven algorithm: determine the MSA target, assess lesion morphology with intravascular imaging, decide whether you need debulking or modification (or both), and then select the device(s) to achieve that goal. In many cases of Complex Angioplasty india Rotablation in india a combination of laser, rotablation/orbital atherectomy and IVL provides the best pathway to optimal stent expansion.
Remember these final points: obtain good imaging up front, avoid creating dissections before debulking, use laser to enable crossing when devices cannot pass, be patient with orbital or rotational passes to reach desired lumen, and employ IVL when deep abluminal calcium is the limiting factor. The modern practice of complex PCI is about device synergy rather than a single-tool orthodoxy — especially in centers and operators performing Complex Angioplasty india Rotablation in india .
Thank you for reading. If you are practicing complex coronary interventions, aim for reproducible MSA endpoints and be comfortable combining tools when a single modality won’t suffice. Complex Angioplasty india Rotablation in india is often best managed with a flexible, imaging-guided, multimodality approach.