 28 April, 2025
28 April, 2025
Back from the Dead: The Astonishing Story of a Heart Attack Patient | Dr AB Gopalamurugan
Heart attacks and sudden cardiac arrests are among the most terrifying medical emergencies one can face. The abrupt cessation of heart function can lead to death within minutes, leaving families and medical teams racing against time to save lives. Yet, modern medicine, advanced technology, and dedicated healthcare professionals have made it possible to bring patients back from the brink of death, restoring not just life but quality of life. This is the extraordinary story of a 35-year-old woman who was clinically dead for two hours but was brought back to life and made a full recovery. It is a testament to the power of swift action, cutting-edge medical intervention, and relentless teamwork.
As the Director of TAVR & Endovascular Therapy, Electrophysiology & Device Therapy, and Senior Consultant in Interventional Cardiology and Electrophysiology at MGM Healthcare, I have witnessed many incredible medical journeys. But this case stands out not only for the clinical complexity but for the human story behind it. Today, I will share this remarkable journey—from the moment she collapsed to her full recovery—highlighting the crucial lessons about cardiac arrest, emergency response, and the miracles that modern medicine can achieve.
The Sudden Collapse: When Heart Failure Strikes Without Warning
Imagine being perfectly healthy and suddenly experiencing a catastrophic failure of your heart. This is precisely what happened to the patient in question. At just 35 years old, with no prior heart disease, she suffered a sudden and severe cardiac arrest. Her heart stopped beating effectively, and she was technically dead.
The initial moments following a cardiac arrest are critical. Each minute without effective circulation causes irreversible damage to the brain and other vital organs. In her case, the situation was dire. We were performing continuous cardiopulmonary resuscitation (CPR) to keep oxygenated blood flowing to her organs. Despite the grim circumstances, the medical team remained focused and determined.
During this time, I was in the middle of a surgery. When the emergency call came through, I immediately instructed the nurse to connect me to the cardiology expert, Dr AB Gopalamurugan, who was essential for the next phase of the patient’s care. Despite the urgency, another doctor, Dr. Sund, was attending another critical patient but still managed to assist remotely.
Racing Against Time: Coordinated Emergency Response
One of the most remarkable aspects of this case was the rapid and coordinated response involving multiple teams and agencies. After finishing the surgery, I quickly prepared the patient for transfer by ensuring all necessary equipment and medications were ready and loaded into an ambulance. The clock was ticking.
Thanks to the extraordinary cooperation of the local police, we secured a “blue light pathway,” allowing the ambulance to cut through city traffic at unprecedented speed. What would normally take much longer was accomplished in just 18 minutes. This swift transport was crucial in getting the patient to a specialized center capable of providing advanced cardiac care.
Arrival and Assessment: The Heart’s Silent Cry
Upon arrival at the hospital, the situation was grim. The patient’s heart showed no contractions—it was as if it had completely shut down. At this stage, traditional resuscitation efforts were insufficient. We needed to take over the function of her heart and lungs artificially to buy more time for diagnosis and treatment.
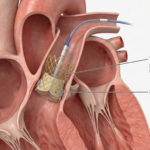
Extracorporeal Membrane Oxygenation (ECMO): The Lifesaving Machine
We employed a highly specialized machine called ECMO (Extracorporeal Membrane Oxygenation). This technology functions as an artificial heart and lung, oxygenating the blood and circulating it throughout the body. ECMO essentially bought us precious time to stabilize the patient and conduct further tests to identify the root cause of her heart failure.
ECMO is a complex and resource-intensive therapy, requiring a skilled team of doctors, nurses, and technicians to monitor and manage the patient around the clock. In this case, our team of 60 dedicated staff members worked tirelessly to ensure the patient’s stability and recovery.
Diagnosing the Cause: The Viral Culprit
With the patient’s heart and lungs supported mechanically, we conducted a battery of tests to uncover why this healthy young woman’s heart had failed so suddenly. After thorough investigation, we identified the cause: a viral infection had attacked her heart muscle, causing severe inflammation and acute heart failure.
Viral myocarditis, as this condition is called, can be unpredictable and devastating. It can affect anyone, regardless of age or prior health status. This diagnosis was a turning point—it allowed us to tailor the treatment specifically to her needs.
The Treatment Journey: Steroids and Supportive Care
Once the diagnosis was established, we began treatment with steroids to reduce inflammation and help the heart muscle recover. However, the road to recovery was long and challenging. The biggest hurdle was to restore the function of her organs to normal. This involved not just cardiac support but also managing other systems affected by the prolonged lack of circulation and oxygen.
Throughout this period, the patient was kept in a medically induced hypothermic state, where her body temperature was artificially reduced to 30°C. This technique helps protect the brain and other organs by slowing metabolic processes and reducing damage during critical illness.
The combination of advanced technology, expert medical care, and constant monitoring allowed her body the chance to heal. Progress was slow but steady, with daily updates provided to her family, who remained hopeful throughout.
The Awakening: From Blank Memory to Full Recovery
For the patient, the experience was surreal. Upon waking, she had no memory of what had happened during those critical hours and days. She described a blankness, a void where time seemed to stretch endlessly. Each minute felt like an hour; every day felt like a year.
It was only after nearly three weeks that she began to regain awareness and sensation. Seeing her husband and parents around her was a pivotal moment, helping her reconnect with reality and begin the emotional journey of recovery.
About a week after waking, her children visited her for the first time. This reunion was a profound milestone—almost 30 days after her cardiac arrest, she finally felt truly alive again.
Returning to Normal Life: A Testament to Modern Medicine
Today, I am proud to say that not only did we bring her back to life, but we also restored her to her old self. She returned to her family, her daily routines, and her dreams—proof that with the right care, even the most severe cardiac emergencies can have hopeful outcomes.
Lessons Learned: The Importance of Immediate Action and Advanced Care
This case highlights several crucial lessons for both the public and healthcare providers:
- Cardiac Arrest Is a Race Against Time: Every minute without effective heart function risks permanent brain damage or death. Immediate CPR and rapid emergency response save lives.
- Advanced Technology Makes a Difference: Machines like ECMO can take over vital functions temporarily, buying time for diagnosis and treatment.
- Collaboration Is Key: The seamless coordination between surgeons, cardiologists, emergency responders, and police ensured swift transport and care.
- Viral Myocarditis Can Affect Anyone: Even healthy individuals are at risk, underscoring the need for awareness and timely medical evaluation if symptoms arise.
- Family Support and Communication Matter: Regular updates and emotional support are vital for patient and family resilience during prolonged critical illness.
What You Should Do If Someone Has a Cardiac Arrest
One of the most powerful takeaways from this story is the importance of immediate action. If you witness someone collapse or suspect a heart attack or cardiac arrest, do not hesitate:
- Call emergency services immediately.
- Start CPR if you are trained; chest compressions can keep blood flowing until professional help arrives.
- Use an Automated External Defibrillator (AED) if available, as early defibrillation can restore a normal heart rhythm.
- Stay with the person and provide reassurance until emergency responders take over.
Remember, by calling for help and initiating early CPR, you can only improve the chances of survival and recovery. The difference you make in those first critical minutes can be life-saving.